Okuqukethwe
eqhubekayo yomdlavuza wesikhumba
Singahlukanisa i- eqhubekayo yomdlavuza wesikhumba ngezigaba ezimbili eziyinhloko: ama-non-melanomas nama-melanomas.
Ama-non-melanomas: ama-carcinomas
Igama elithi "carcinoma" lichaza izicubu eziyingozi zemvelaphi ye-epithelial (i-epithelium iyisakhiwo somlando wesikhumba kanye nolwelwesi oluthile).
I-Carcinoma uhlobo lwe umdlavuza otholakala kakhulu kubantu baseCaucasus. Kukhulunywa kangako ngoba akuvamile ukuthi kuphumele ekufeni. Ngaphezu kwalokho, kunzima ukubona amacala.
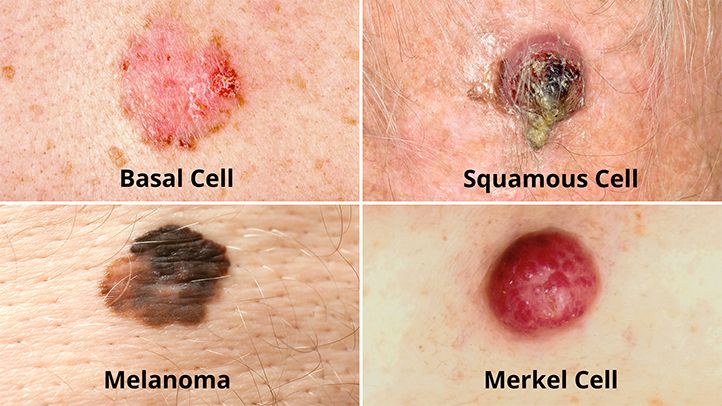
Le basal cell carcinoma futhi i-squamous cell carcinoma noma i-epidermoid yizinhlobo ezi-2 ezivame kakhulu ze-non-melanoma. Imvamisa zenzeka kubantu abaneminyaka engaphezu kwengama-50.
I-Carcinoma iseli eliyisisekelo kukodwa kwakha cishe Ama-90% omdlavuza wesikhumba. Yakha ungqimba olujulile lwe-epidermis.
E-Caucasians, i-basal cell carcinoma akuyona nje umdlavuza wesikhumba ovame kakhulu, kodwa umdlavuza ovame kakhulu kuwo wonke umuntu, omele u-15 kuya ku-20% wawo wonke umdlavuza eFrance. Ubungozi be-basal cell carcinoma empeleni bukhona (cishe abusoze buholele kuma-metastases, izicubu zesibili ezakha kude nesimila sokuqala, ngemuva kokuthi amangqamuzana omdlavuza ahlukanisiwe nawo), okwenza ukuthi kungavami ukubulala, kepha ukuxilongwa kwawo sekwephuze kakhulu , ikakhulukazi ezindaweni ze-perioriform (amehlo, impumulo, umlomo, njll.) Kungakhubaza umzimba, kubangele ukulahleka okukhulu kwento yesikhumba.
I-Carcinoma sphamandla ou epidemoid iyi-carcinoma eyenziwa ngokukhishwa kwe-epidermis, ekhiqiza ukubonakala kwamaseli we-keratinized. EFrance, ama-epidermoid carcinomas eza endaweni yesibili phakathi komdlavuza wesikhumba futhi amele cishe ama-20% we-carcinomas. Ama-squamous cell carcinomas angadlalisa umzimba kepha lokhu akuvamile futhi yi-1% kuphela yeziguli ezine-squamous cell carcinoma ezibulawa ngumdlavuza wazo.
Kukhona ezinye izinhlobo ze-carcinoma (adnexal, metatypical…) kepha zehlukile impela
I-Melanoma
Sinikeza igama le-melanoma ku- izimila ezimbi akha ama-melanocyte, amaseli akhiqiza i-melanin (i-pigment) etholakala ikakhulukazi esikhumbeni nasemehlweni. Imvamisa zibonakalisa njenge ibala elimnyama.
Ngamacala amasha ama-5 alinganiselwa eCanada kuma-300, i-melanoma imele i- 7e umdlavuza okutholakala kakhulu ezweni11.
The melanoma kungenzeka nganoma yisiphi isikhathi. Aphakathi komdlavuza ongathuthuka ngokushesha futhi ukhiqize ama-metastases. Babhekene nama-75% we ukufa kubangelwa umdlavuza wesikhumba. Ngenhlanhla, uma zitholakala kusenesikhathi, zingelashwa ngempumelelo.
Amanothi. Esikhathini esedlule, bekukholelwa ukuthi kungaba nama-melanomas (ama-tumors achazwe kahle angenakwenzeka ukuthi ahlasele umzimba) nama-melanoma amabi. Manje sesiyazi ukuthi wonke ama-melanoma ayingozi.
Izimbangela
Ukuchayeka ku imisebe ye-ultraviolet du sun imbangela enkulu ye- eqhubekayo yomdlavuza wesikhumba.
Imithombo yokufakelwa yemisebe ye-ultraviolet (amalambu elanga ku- nokucwilisa nokucwala) nazo ziyabandakanyeka. Izingxenye zomzimba ezivame ukuvezwa yilanga yizona ezisengozini enkulu (ubuso, intamo, izandla, izingalo). Noma kunjalo, umdlavuza wesikhumba ungakha noma kuphi.
Ngezinga elincane, ukuxhumana isikhathi eside kwesikhumba ne- imikhiqizo yamakhemikhali, ikakhulukazi emsebenzini, ingandisa ingozi yokuba nomdlavuza wesikhumba.
Ukushiswa yilanga nokuchayeka njalo: qaphela! Ukuvezwa yimisebe ye-ultraviolet ine imiphumela ekhulayo, okusho ukuthi, ziyahlanganiswa noma zihlanganiswe ngokuhamba kwesikhathi. Ukulimala kwesikhumba kuqala esemncane futhi, yize kungabonakali, kuyanda kuyo yonke impilo. I- umdlavuza (ama-non-melanomas) adalwa kakhulu wukuchayeka elangeni kaningi nangokuqhubekayo. I- melanoma, kwabo, ikakhulukazi kubangelwa ukuvezwa okunamandla nokufushane, ikakhulukazi lezo ezibangela ukushiswa yilanga. |
Izinombolo:
- Emazweni lapho iningi labantu likhona Isikhumba esimhlophe, amacala omdlavuza wesikhumba asengozini ye- double phakathi konyaka ka-2000 nonyaka ka-2015, ngokusho kombiko weZizwe Ezihlangene (UN)1.
- ECanada, luhlobo lomdlavuza olukhula ngokushesha, lukhula ngo-1,6% unyaka nonyaka.
- Kulinganiselwa ukuthi ngama-50% abantu abavela phezu 65 bazoba nomdlavuza wesikhumba okungenani owodwa ngaphambi kokuphela kwempilo yabo.
- Umdlavuza wesikhumba uhlobo oluvame kakhulu lwe umdlavuza wesibili : ngalokhu sisho ukuthi umuntu onomdlavuza noma onomdlavuza kungenzeka abe nomunye, ngokuvamile umdlavuza wesikhumba.
kwesifo
Okokuqala kunakho konke a ukuhlolwa ngokomzimba okuvumela udokotela ukuthi azi ukuthi ngabe ukulimala kungenzeka noma ungabi nomdlavuza.
I-Dermoscopie : lokhu ukuhlolwa ngohlobo lwengilazi yokukhulisa ebizwa nge-dermoscope, ekuvumela ukuthi ubone ukwakheka kwezilonda zesikhumba nokwenza ngcono ukuxilongwa kwabo.
i-biopsy. Uma udokotela esola umdlavuza, uthatha isampula yesikhumba endaweni yokubonakaliswa okusolisayo ngenhloso yokuyithumela kohlaziyo lwelabhoratri. Lokhu kuzomvumela ukuthi azi ukuthi isicubu sinomdlavuza ngempela yini futhi kuzomnika umbono wesimo sokuqhubekela phambili kwalesi sifo.
Okunye ukuhlolwa. Uma i-biopsy ikhombisa ukuthi isihloko sinomdlavuza, udokotela uzo-oda ezinye izivivinyo ukuze aqhubeke nokuhlola isigaba sokuqhubeka kwesifo. Ukuhlolwa kungasho ukuthi umdlavuza usalokhu ukhona noma ngabe usuqale ukusabalala ngaphandle kwezicubu zesikhumba.