Okuqukethwe
I-Cholangiocarcinome
Kwenzenjani ?
I-Cholangiocarcinoma umdlavuza we-bile ducts. Kuthinta i-epithelium yesihlahla se-biliary se-intra noma se-hepatic eyengeziwe, okusho ukuthi izicubu ezakhiwe amaseli ahlangene asondelene akha isethi yamashaneli aqoqa i-bile. I-Bile iwuketshezi oluphuzi lwe-viscous olukhiqizwa isibindi, ngakho-ke amathuba okuba nesifo se-intra noma se-hepatic eyengeziwe.
Naphezu kokusakazeka okuncane kwalesi sifo okwaziwayo, i-cholangiocarcinoma yenza cishe u-3% womdlavuza wamathumbu kanye ne-10 kuya ku-15% ye-hepato-biliary malignancies. Kukhona ukudlondlobala okuncane kwabesilisa ekuthuthukisweni kwalesi sifo. Ngaphezu kwalokho, lesi sifo sikhula ngokwesilinganiso phakathi kweminyaka engama-50 nengama-70.
Imvelaphi yokuthuthukiswa kwalesi simila ayikacaci. Noma kunjalo, kubonakala sengathi ukwenzeka kwayo akuvamile, okusho ukuthi kuthinta kuphela abantu abathile phakathi kwabantu ngaphandle kokuba khona “kochungechunge lokudlulisela” oluchaziwe. (1)
Lo mdlavuza ungakhula ngo:
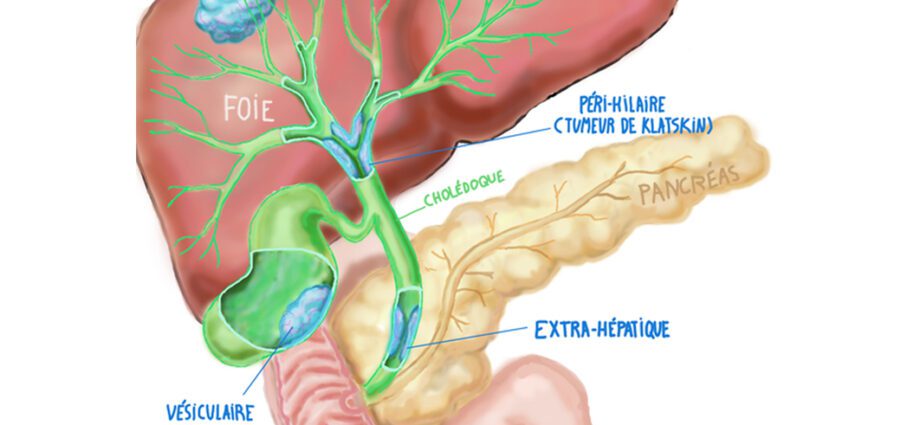
- i-intrahepatic bile ducts. Lezi zindlela zenziwe ngamapayipi amancane (canaliculi), ama-Herring ducts nama-bile ducts. Le sethi yamashaneli ihlangana ndawonye ukuze yakhe isiteshi esivamile kwesokunxele nesokudla. Lezi zishiya isibindi ukuze zenze umgudu ovamile we-extrahepatic. Uhlobo oluthile lwesimila oluthinta ukuhlangana phakathi kwemigudu ye-hepatic kwesokudla nesobunxele lubizwa ngokuthi: Isimila sikaKlatskin;
- i-extrahepatic bile ducts, eyenziwe ngomgudu omkhulu we-bile kanye ne-accessory bile duct.
Izimpawu ezihambisana nalolu hlobo lomdlavuza zihlukile kuye ngomonakalo ongaphakathi noma owengeziwe wesibindi. Ngaphezu kwalokho, ukubonakaliswa komtholampilo kuvame ukuvela lapho lesi sifo sisezingeni eliphezulu lokukhula kwaso.
Kuyisifo esingavamile esinezigameko zomuntu oyedwa kwabayi-1. (100)
Izimpawu
Izimpawu zesifo zivela esiteji esiphezulu futhi zihlukile kuye ngokuthi indawo yesimila.
Ngempela, esimweni lapho isimila singaphezu kwesibindi, izimpawu ezihambisanayo yilezi: (1)
- ukubonakaliswa kwe-cholestatic: indle ecacile, i-jaundice, umchamo omnyama, i-pruritus, njll.
- ukungakhululeki;
- ukunciphisa umzimba;
- umuzwa wokukhathala nobuthakathaka.
Esimweni sokubandakanyeka kwe-intrahepatic, lesi sifo sichazwa kakhulu ngokuphatheka kabi kanye nezimpawu ezithile zesisu ezifana nalezi:
- ukunciphisa umzimba;
- i-anorexia;
– ubuhlungu besisu.
Ezinye izimpawu zingahlotshaniswa nalesi sifo: (2)
- imfiva ;
- ukulunywa;
– ubuhlungu engxenyeni engenhla kwesokudla sesisu.
Lesi sifo sichazwa ngezigaba eziningana: (3)
- isigaba 1a: umdlavuza utholakala ngaphakathi kwe-bile ducts;
- isigaba 1b: umdlavuza uqala ukusabalala futhi usakazeke emithanjeni ye-lymphatic;
- isigaba 2: umdlavuza uqala ukusabalala ngezicubu (ikakhulukazi isibindi) kanye nemithambo ye-lymphatic;
- isigaba sesi-3: umdlavuza ukhona ngendlela ye-metastatic eningi legazi nemithambo ye-lymphatic;
– isigaba 4: umdlavuza usabalele kuzo zonke izitho zomzimba.
Imvelaphi yalesi sifo
Imbangela eqondile yomdlavuza wenyongo, kuze kube namuhla, ayikaziwa. Kodwa-ke, izici eziyingozi zokuthuthukiswa kwe-cholangiocarcinoma ziqondwa kangcono.
Umdlavuza uvela ekuguqulweni kwezakhi ngaphakathi kwesithwali solwazi lofuzo lwamaseli: i-DNA.
Lokhu kuguqulwa kofuzo ngaphakathi kwamangqamuzana kuholela ekwandeni kokukhula kanye nokukhula okungalawuleki kwamangqamuzana okuholela ekwakhekeni kwesigaxa seseli esibizwa ngokuthi isimila.
Esimeni lapho umdlavuza ungatholakali ngesikhathi futhi/noma ungelashwa ngokushesha, isimila singakhula sibe sikhulu futhi sisakazekele kwezinye izingxenye zomzimba noma by ukugeleza kwegazi. (3)
I-Cholangiocarcinoma ibonakala ngesimila esithinta i-bile ducts. Lokhu kuvame ukukhula kancane futhi ukuvela kwayo kusimo se-metastatic nakho kuhamba kancane.
Ngaphezu kwalokho, ukuhlolelwa lesi sifo kuvame ukwenziwa esigabeni esithuthukile sesimila.
Isimila singakhula kunoma yiliphi izinga eduze kwe-bile duct futhi sivimbele ukugeleza kwe-bile.
Izici zengozi
Nakuba umsuka oqondile walesi sifo uwukuthi, kuze kube namuhla, namanje akwaziwa, izici eziningi zobungozi ezihlobene nalesi sifo zicacile. Lokhu kunjalo ikakhulukazi: (2)
- ukuba khona kwama-cysts ku-bile ducts;
- ukuvuvukala okungapheli kwe-bile ducts noma isibindi;
- i- primary and secondary sclerosing cholangitis (ukuvuvukala kwe-necrotizing yama-bile ducts okubangela ukuba abe mncane futhi aphazamise ukugeleza okuvamile kwe-bile);
- i-ulcerative colitis (isifo esingapheli sokuvuvukala kwamathumbu amakhulu);
- isifo se-typhoid esingamahlalakhona (ukuthuthukiswa kwemfiva ye-typhoid umsuka wayo uvela esikhumbeni esithathelwanayo futhi esingadluliselwa komunye umuntu kuya komunye);
- izifo ze-parasitic by I-Opisthochis viverrini i-pair I-Clonorchis sinensis;
- ukuchayeka ku-thorotrast (i-ejenti yokuqhathanisa esetshenziswa kuma-x-ray radiographs).
Ezinye izici zomuntu siqu nazo ziyavela ekukhuleni kwalolu hlobo lwesimila: (3)
- iminyaka yobudala; abantu abangaphezu kweminyaka engama-65 basengozini enkulu yokuthola lesi sifo;
- ukuchayeka kumakhemikhali athile. Ukuchayeka ku-thorotrast yisibonelo esihle kakhulu. Ngempela, kuye kwafakazelwa ukuthi ukuchayeka kule agent yamakhemikhali esetshenziswa kabanzi ku-radiography, ngaphambi kokuvinjelwa kwayo ngawo-1960, kwandisa ingozi yokuthuthukisa i-cholangiocarcinoma. Amanye amakhemikhali nawo ahilelekile ekwandiseni ingozi yokuthola lesi sifo, njenge-asbestos noma ama-PCB (i-polychlorinated biphenyls). Eyokuqala yasetshenziswa isikhathi eside njengento evimbela ilangabi emikhakheni yokwakha, yokwakha kanye nezimboni. Ama-PCB nawo avame ukusetshenziswa ezimbonini nasezokwakha. Lawa makhemikhali manje angaphansi kwemithetho eqinile;
- ukuba khona kwe-hepatitis B noma C;
- ukuba khona kwe-cirrhosis;
- ukutheleleka nge-HIV (i-Human Immunodeficiency Virus);
- uhlobo I nohlobo II sikashukela;
- ukukhuluphala;
- ugwayi.
Ukuvimbela nokwelashwa
Ukuhlolwa okuhlukile kokuhlolwa komdlavuza wemigudu yenyongo kufanele kwenziwe ukuze kutholakale isifo. (3)
- ukuhlolwa kwegazi kusetshenziselwa ukuxilongwa kwe-cholangiocarcinoma. Eqinisweni, esimweni lapho kuvela khona isimila emiseleni yenyongo, amangqamuzana omdlavuza akhulula amakhemikhali athile angabonakala ngokuhlolwa kwegazi. Nokho, lezi zimaki zingakhululwa ngaphansi kwezinye izimo. Ukuba khona kwalezi zinto akuhambisani ngokuhlelekile nokuthuthukiswa komdlavuza we-bile ducts;
- isithwebuli se-bile ducts senza kube lula ukuthola isithombe sengaphakathi lale ngxenye yomzimba ukuze kutholwe noma yikuphi ukungahambi kahle;
- i-tomography, ngokusebenzisa uchungechunge lwe-X-ray yesibindi, ivumela ukuhlaziywa okuningiliziwe kwalesi sitho ngezithombe ezi-3-dimensional;
- I-MRI (I-Magnetic Resonance Imaging), isebenzisa uhlelo lwamagnetic field namaza omsakazo ukuthola isithombe sengaphakathi lesibindi;
- i-retrograde cholangiopancreatography i-endoscopy iyindlela yokugqamisa ukungahambi kahle okuningiliziwe kwamapayipi enyongo;
- i-percutaneous transhepatic cholangiography iphinde isetshenziselwe ukuthola ukubuka kabanzi kwe-gallbladder;
- i-biopsy ivumela ukuqinisekiswa kokuxilongwa.
Izimo eziningi zomdlavuza we-bile duct azikwazi ukwelapheka. Kodwa-ke, ukwelashwa kwalesi sifo kuvame ukuhambisana nezimpawu ezithile.
Ukulandelelwa kwesiguli kwenziwa ngenxa yethimba lemikhakha eminingi elakhiwe iqoqo lochwepheshe (odokotela abahlinzayo, i-oncologist, i-radiologist, abahlengikazi, i-gastroenterologist, njll.). (3)
Ukwelashwa okunikezwayo kuncike ezimpawu kanye nokuqhubeka komdlavuza.
Ezigabeni 1 no-2, ukuhlinzwa kungenzeka ukuze kuvuselelwe ingxenye yenyongo, imigudu yenyongo noma isibindi.
Esigabeni sesi-3, amathuba okuphumelela kokwelashwa ancike ezingeni lomonakalo emithanjeni ye-lymphatic.
Ekugcineni, esigabeni sesi-4, izinga lempumelelo yokwelashwa liphansi uma kuqhathaniswa.
Ukwelashwa kwalesi sifo kungabangela ukungenelela kokuhlinzwa okuvumela ukuvuselelwa kwezicubu ezinomdlavuza: ingxenye yemigudu ye-bile equkethe amangqamuzana omdlavuza, i-gallbladder, imikhumbi ethile ye-lymphatic ethintekile noma ngisho nengxenye yesibindi.
Ngokuvamile, phakathi kuka-20% no-40% wabantu abahlinzwa futhi bahlinzwa baphila iminyaka engu-5 noma ngaphezulu ngemva kokuhlinzwa.
Ngokumelene nesizinda sobuhlungu besisu, i-jaundice, njll., ukuvuleka kwe-bile ducts ngezinye izikhathi kuyadingeka. Lokhu kukhululwa kwenziwa kusetshenziswa ishubhu elincanyana elidlula emiseleni yenyongo.
Ukwelashwa ngemisebe akuyona indlela evamile yokwelapha i-cholangiocarcinoma, nokho kungasebenza ekwehliseni izimpawu kanye nasekunciphiseni ukusakazeka kwama-metastase. Kunezinhlobo ezimbili zokwelashwa ngemisebe: ukwelashwa ngemisebe yangaphandle kanye nokwelashwa ngemisebe yangaphakathi.
Ngaphezu kwalokho, i-radiotherapy ingabangela imiphumela engemihle njengokucanuzela kwenhliziyo, ukuhlanza noma ngisho nokukhathala okukhulu.
I-Chemotherapy iphinde isetshenziselwe izinjongo ezifana nokwelapha ngemisebe. Noma ukuze kuncishiswe izimpawu, ukuze kuncishiswe ukusabalala kwesimila futhi kwandise isikhathi sokuphila sesihloko esithintekile. I-Chemotherapy ivame ukuhlanganiswa ne-radiotherapy. Imiphumela engemihle ehambisana ne-chemotherapy nayo ihlotshaniswa ne-radiotherapy kanye nokulahlekelwa izinwele.
Olunye ucwaningo lubonise izinzuzo ezihambisana nokuhlanganiswa kwezidakamizwa ezimbili ezisetshenziswa ku-chemotherapy (i-Cisplatin ne-Gemcitabine).
Kuze kube manje, ukwelashwa okuhlotshaniswa nomdlavuza we-bile ducts akuphumelelanga njengalezo ezihlotshaniswa nezinye izinhlobo zomdlavuza. Ngakho-ke, izifundo eziningi zigxile kulolu hlobo lomdlavuza ukuze kutholwe izindlela ezingcono zokwelapha lesi sifo.
Ngaphezu kwalokho, ucwaningo ekuthuthukisweni kwezindlela zokwelapha ezihlosiwe nalo lukhona manje. Lezi yizidakamizwa ezikhomba isigaba esithile ekuthuthukisweni komdlavuza.